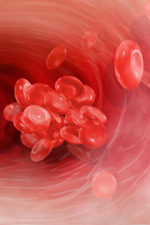
The attorneys at Prieto, Marigliano, Holbert & Prieto, LLC. have litigated numerous malpractice cases for clients who suffered severe bleeding complications related to a commonly prescribed anti-coagulant or blood thinner called warfarin or Coumadin. Warfarin is the most commonly used oral anticoagulant in the US. An anticoagulant is a drug used to prevent unwanted and dangerous blood clots. Although anticoagulants are often called “blood thinners,” warfarin does not actually make your blood thinner. Warfarin interferes with the body’s ability to make a blood clot. Warfarin is also sold as Coumadin and Jantoven, which are brand names for the generic drug warfarin. This medication is prescribed for many medical conditions that increase a patient’s risk for forming potentially fatal blood clots like deep vein thrombosis (DVT) or arterial fibrillation.
How does warfarin work?
In order for your blood to form a clot, you have to have certain proteins in your blood. Normally, your liver makes these proteins and it requires vitamin K to do so. You get vitamin K from many of the foods you eat (especially green vegetables and certain oils). Warfarin reduces your liver’s ability to use vitamin K to make these blood clotting proteins, which makes it harder for your blood to clot. Vitamin K and warfarin tend to work against each other. For this reason warfarin is often referred to as a vitamin K antagonist (VKA). If your intake of vitamin K increases, you will need more warfarin to keep your blood from clotting. If your intake of vitamin K is reduced, your dose of warfarin will also have to be reduced in order to keep you from bleeding. Fortunately, both the amount of vitamin K and warfarin in your body tends to rise and fall somewhat slowly. Therefore, one way to think about this balance between warfarin and vitamin K is that it is the WEEKLY (rather than the daily) intake that is being balanced against each other. Additionally, because the level of warfarin rises or falls rather slowly, any change in dose may take several days or even a few weeks to reach a new stable level. Similarly, if you miss a dose of warfarin (or take an extra dose) the level of warfarin (and therefore its effect) may be altered for several days.
Overdose? Did it Happen to You?
The most important effect of a Coumadin overdose is bleeding. This can include obvious bleeding, such as vomiting of blood, nosebleeds or bright red blood in the stool or bleeding that is less obvious, such as internal bleeding. Signs of an overdose might include:
- Easy bruising
- Cuts or scrapes that are slow to stop bleeding
- Signs of gastrointestinal bleeding, such as:
- Black, tarry stools
- Bright red blood in the stool
- Vomiting of blood
- Signs of a hemorrhagic stroke (bleeding in the brain) or a subdural hematoma, such as:
- Vision or speech changes
- Weakness or numbness in an arm or leg
- Severe headache
An overdose of Coumadin can occur in several different ways. If you are or a loved one thinks that he/she has been over-dosed or sustained an injury while on warfarin, call us now to discuss your rights and what we can do to help.
